Why This Matters More Than You Think
If you or someone you love is using opioids—whether prescribed or not—one of the most common and important questions is: How long do opioids stay in your system? It’s not just a matter of curiosity. This question carries real-world weight in situations like:
- Preparing for a drug test
- Starting a treatment program
- Monitoring pain medication use
- Trying to support a loved one in recovery
Understanding how opioids move through the body helps people make informed choices, stay safe, and seek the right kind of support when needed. And if you’re in recovery—or thinking about it—knowing how long these substances linger can be the first step toward accountability and healing.
Opioids don’t affect everyone the same way. Factors like what type of opioid you took, how often you’ve used it, and even your metabolism can all affect how long it stays in your system. But before we dive into those details, let’s take a closer look at the different types of opioids and how they work in the body.

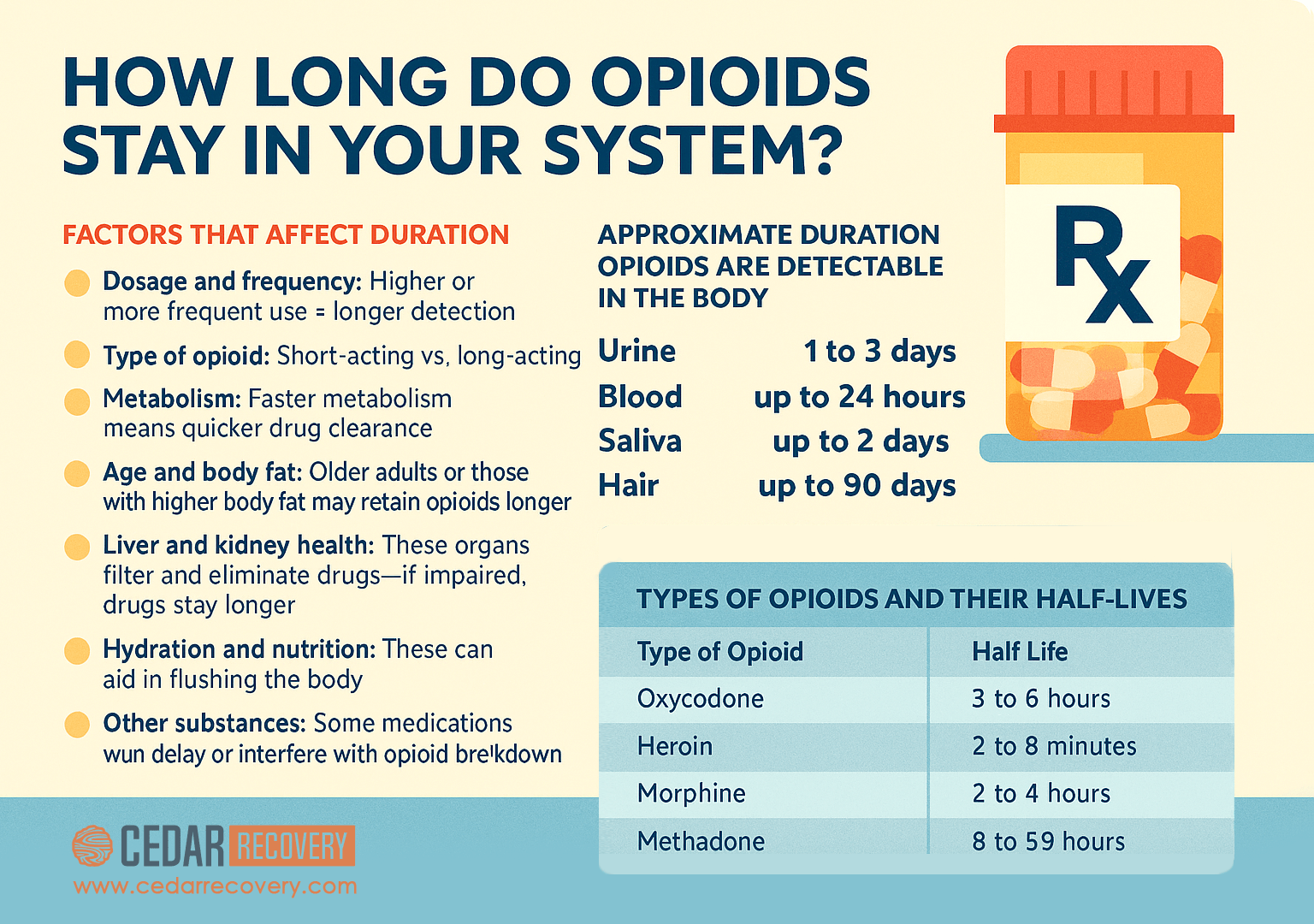
Types of Opioids and Their Half-Lives
Opioids come in many forms, from short-acting pills to long-lasting patches. Here’s a breakdown of commonly used opioids and how long they generally remain active in the body:
The term half-life refers to how long it takes for half of the drug to be eliminated from your body. Just because the drug’s effects may wear off doesn’t mean it’s completely gone. Many opioids break down into metabolites—chemical byproducts—that can linger in the body and show up in tests.
How the Body Processes Opioids
Once opioids enter your body—whether through a pill, injection, or patch—they begin a complex journey through your bloodstream. Here’s how the process typically works:
- Absorption: After use, opioids are absorbed into the bloodstream and start interacting with the brain’s opioid receptors, leading to pain relief, euphoria, or sedation.
- Metabolism: The liver processes the drug and breaks it down into metabolites. These metabolites are what drug tests often detect.
- Excretion: Finally, the body eliminates opioids through urine, stool, sweat, and in some cases, saliva or breath.
This entire process can be influenced by your age, health, metabolism, hydration level, and even other medications you’re taking.
Drug Testing Methods and Detection Windows
There’s no single answer to “how long do opioids stay in your system,” because detection varies based on the testing method used. Here’s what to expect:
1. Urine Testing
The most common method typically detects:
- Short-acting opioids: 1–3 days
- Long-acting opioids (like methadone): up to 7 days
- Fentanyl: 24–72 hours
- Heroin: up to 3 days
2. Blood Testing
Less common and has a shorter window:
- Most opioids: detectable for a few hours up to 24 hours
- Fentanyl/Heroin: often clears within 12 hours
3. Saliva Testing
Simple and non-invasive: Most opioids are detected for 1–2 days after use
4. Hair Testing
Longest detection window: All opioids: up to 90 days, depending on length of hair and frequency of use
Factors That Affect How Long Opioids Stay in Your System
Every person processes opioids a little differently, which is why the timeline for how long opioids stay in your system can vary so much. Here are several key factors that can influence detection times and overall drug clearance:
1. Dosage and Frequency of Use
The more often and the more heavily you use opioids, the longer they tend to remain in your body. A single prescribed dose for post-surgery pain might clear in a day or two, but long-term or high-dose use builds up in your system. This cumulative effect can significantly extend the time opioids are detectable in drug tests.
2. Type of Opioid Used
Short-acting opioids like oxycodone or hydrocodone are metabolized more quickly, while long-acting opioids like methadone or extended-release morphine stay in the system much longer. Fentanyl, while potent, has a shorter half-life when injected but may linger if used via a patch. Each opioid has unique properties that impact metabolism and detection.
3. Metabolism Rate
Your body’s metabolism plays a major role in drug elimination. People with faster metabolic rates may process and excrete opioids more efficiently. This can be influenced by genetics, physical activity, and overall health. If your metabolism is slower, due to age, certain conditions, or lifestyle factors, opioids may linger longer in your system.
4. Age and Body Fat Composition
As we age, our metabolic processes tend to slow down, which can cause drugs to remain in the body longer. In addition, opioids are fat-soluble, meaning they can be stored in fatty tissue. Individuals with higher body fat percentages may retain traces of opioids for a longer period, especially with repeated use.
5. Liver and Kidney Health
Your liver and kidneys are responsible for filtering, breaking down, and excreting drugs. If either organ is impaired—even slightly—opioid metabolism can slow down, extending how long the drug stays in your system. This is especially important for people with chronic liver disease or kidney conditions.
6. Hydration and Nutrition
Staying hydrated helps your kidneys function properly, which can aid in clearing opioids from your body. Likewise, good nutrition supports your overall metabolism. Poor hydration or malnutrition can delay detoxification and make withdrawal symptoms feel more intense.
7. Use of Other Substances or Medications
Certain medications can either speed up or slow down the metabolism of opioids. For example, some antidepressants and antifungal drugs interfere with liver enzymes that process opioids. Alcohol or other substances can also complicate metabolism, potentially increasing side effects or overdose risk.
Why This Information Matters in Recovery
Understanding how long opioids stay in the system isn’t just about passing a test. It’s about empowering yourself with knowledge and making safer, healthier choices. Here’s why it matters:
- Preventing opioid overdose: After even short-term abstinence, your tolerance drops. Taking the same dose you used before can lead to an overdose.
- Timing MAT treatment: If you’re transitioning to Medication-Assisted Treatment (MAT), knowing how long opioids stay in your system helps your care team make safer medical decisions.
- Avoiding withdrawal surprises: Understanding timelines can help you mentally and physically prepare for symptoms of withdrawal.
- Supporting recovery goals: Being informed helps you stay grounded and motivated during early recovery.
Treatment and Support Options at Cedar Recovery
Whether you’re still using opioids, actively withdrawing, or years into recovery, Cedar Recovery is here for you. Our approach is rooted in compassion, medical excellence, and long-term healing.
Here’s how we can help with opioid use disorder:
- Medication-Assisted Treatment (MAT): Suboxone and other medications to ease withdrawal and reduce cravings
- Therapy and Counseling: Mental health care that addresses trauma, depression, and anxiety
- Recovery Support: Community partnerships that connect you to people who truly understand
We understand how hard this road can be. But you don’t have to walk it alone.
Healing Begins with Cedar Recovery
We’re here to support you, whether you’re ready for treatment or just need someone to talk to. There’s no shame in asking for help. In fact, it may be the most courageous thing you’ve ever done.
Contact us today or visit one of our Tennessee or Virginia outpatient treatment locations to get started. You are not alone, and you don’t have to carry this by yourself anymore.
Sources:
- National Institute on Drug Abuse. (2023). Drug testing. U.S. Department of Health and Human Services. https://nida.nih.gov/research-topics/drug-testing
- National Institute on Drug Abuse. (2020). Prescription opioids: DrugFacts. U.S. Department of Health and Human Services. https://nida.nih.gov/publications/drugfacts/prescription-opioids
- National Institute on Drug Abuse. (2023). Opioids. U.S. Department of Health and Human Services. https://nida.nih.gov/research-topics/opioids
- Bogen, I. L., Boix, F., Andersen, J. M., Steinsland, S., Nerem, E., & Mørland, J. (2023). Heroin metabolism in human blood and its impact for the design of an immunotherapeutic approach against heroin effects. Basic & Clinical Pharmacology & Toxicology, 133(4), 412–421. https://doi.org/10.1111/bcpt.13926
- PubChem. (n.d.). Methadone. National Center for Biotechnology Information. https://pubchem.ncbi.nlm.nih.gov/compound/Methadone
- MedlinePlus. (2023). Opiate and opioid withdrawal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/000949.htm
- U.S. Food and Drug Administration. (2017). Drugs of abuse home use test. https://www.fda.gov/medical-devices/drugs-abuse-tests/drugs-abuse-home-use-test
- Quest Diagnostics. (2013). Drug half-life, steady state, and recommended sample collection time. https://testdirectory.questdiagnostics.com/test/test-guides/TB_DrugHalfLife/drug-half-life-steady-state-and-recommended-sample-collection-time
- National Institute on Alcohol Abuse and Alcoholism. (2007). Alcohol metabolism: An update. https://www.niaaa.nih.gov/publications/alcohol-metabolism
- Substance Abuse and Mental Health Services Administration. (2021). Chapter 3B: Methadone. In Medications for opioid use disorder: For healthcare and addiction professionals, policymakers, patients, and families (TIP Series No. 63). National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK574918/